This looks like an unspoken epidemic in the UK with the incontinence pads taking up more room in the supermarket than period products. (three sets of shelves to one)

43% of women in the UK in their 50s will suffer and this rises to 51% of women over 65. Main contributory factors are giving birth naturally, menopause and ageing when facia damage and muscle weakness become issues. Chronic constipation, heavy or repeated lifting without correct abdominal bracing, constant coughing eg smokers chronic cough, being very overweight or frequent vigorous high impact exercise may also contribute. It is not solely a female issue but it impacts far fewer men.
There are two main types of urinary incontinence – urge and stress.
Urge incontinence – this is when you are desperate to go to the loo and can’t hold it, this may involve some leaking. Urge is mostly caused by your bladder being irritated by insufficient fluid or by the nature of the fluids consumed. It is also triggered by hormone imbalances during menopause. It is normal for you to urinate 4 to 8 times a day, or every two to three hours. It is also very common to get up once in the night to urinate. If you are constantly up and down in the night, and/or peeing super frequently with desperation, please make an appointment with your GP
If you go more frequently what actions can you take?
You can remove irritants from your diet. This will prove very hard for many as the biggest culprit is caffeine, closely followed by alcohol. Then fizzy drinks, so beer is a bit of an issue! Other irritants are citrus fruits and juices, chocolate because it contains caffeine, green tea and tomatoes. You may be more irritated by some things than others so it is worth testing things out.

You can make sure you drink enough non irritant fluids. We need approximately two litres a day, without factoring in dehydration from exercise. This can include water, milk, decaffeinated drinks, herbal teas, diluted fruit juice (non citrus) and milk shakes. You can also add in there electrolyte drinks, and sports carbohydrate drinks. The sugars in some sports drinks may be irritants for you though, experiment with different brands.
As we become older we lose our thirst mechanism so it becomes more and more of a discipline to drink. ‘I’m not thirsty’ doesn’t cut it.
In menopause HRT and oestrogen pessaries may provide some relief from urinary urges.
Stress incontinence – this is when you leak urine without meaning to. For example when laughing, sneezing, coughing, skipping or running. The most common reason is that the pelvic floor muscles are not functioning correctly. All the bladder, bowel and sexual functions require good pelvic floor function. The pelvic floor muscles are thin bands of muscles in a figure of eight around the anus, urethra and vaginal opening which form a thin sheet of muscle. They support the bladder, uterus and bowels. Like any other muscle in the body they may become weak, overstretched, slow to work, too tight or torn. And just like any other muscle in the body we should look after them by exercising them regularly. But if you are like most humans you will forgot or ignore them as ‘out of sight out of mind’. The time we generally start to think about them is when they stop working properly!
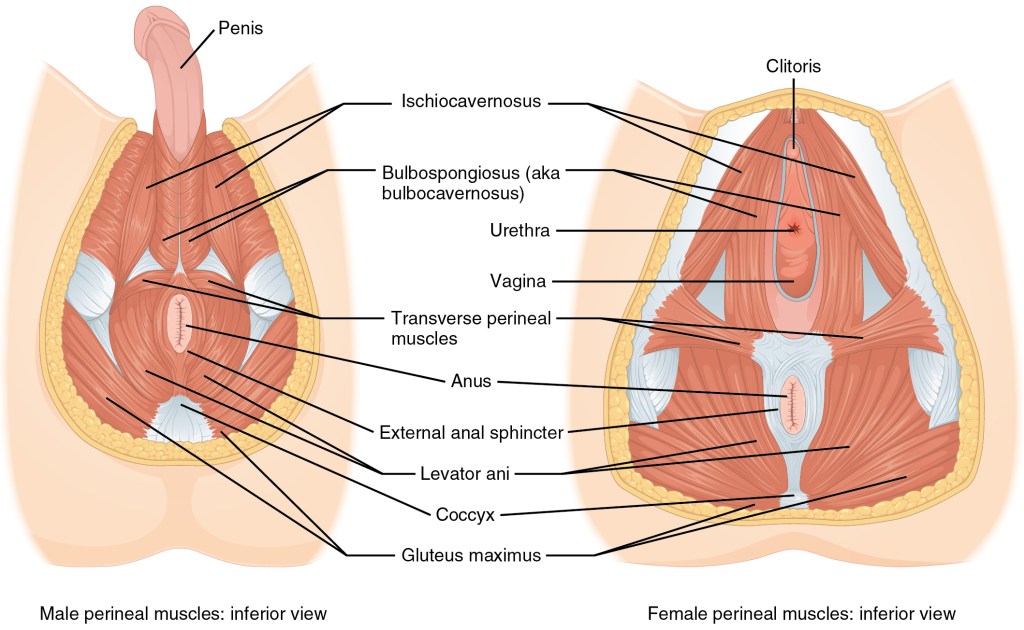
What should we do? We should do pelvic floor exercises daily. This involves tightening your pelvic floor and holding for ten seconds. Do this ten times.
Then quickly tighten them and let go after a couple of seconds, also do this ten times. When doing both exercises relax the pelvic floor completely in between each exercise.
If you don’t know where they are try stopping the flow of urine while you are urinating and be aware of which muscles you are activating. Only do this to get the feel for what your are trying to do, don’t do it regularly. The muscles around the anus should contract as well as the ones at the front of your lower abdomen, just above your pubic bone.
If you are currently experiencing leakage do pelvic floor exercises three times a day for three months. If you are still struggling after this go and see your GP. There are solutions and there is no reason why you should suffer for years. Your GP may prescribe menopause treatment, examine you, to ensure there are no other issues which need treating, and may refer you to an NHS specialist physiotherapist. Taking this course of action may ease embarrassment, self esteem issues and loss of confidence outside of the doctor’s surgery. It might enable you to enjoy things which you have given up due to bladder issues and it may save you a fortune in Tena pads over future years!
Useful contacts – NHS App Squeezy – free
Dr Bri on YouTube – free, her Kegel Camp is good
Buff Muff App – cost attached
https://www.nhs.uk/conditions/urinary-incontinence/
https://my.clevelandclinic.org/health/body/22729-pelvic-floor-muscles
https://www.nuffieldhealth.com/article/how-much-water-should-you-drink-per-day
https://www.health.harvard.edu/staying-healthy/how-much-water-should-you-drink
https://www.wellbeingofwomen.org.uk/health-information/urinary-incontinence/




























 We both lost our three streams of income at once, with no guarantee that they were going to return. We went from a household of two to a household of six. Two adult children arrived home jobless, one bringing a jobless partner, and the third came back to sit online university exams with no guarantee of his third year going ahead. Uncertainly was rife. My husband then returned to hospital with an attack of Atrial fibrillation, a heart condition. Nothing to do with stress!? Things have since calmed down a bit, and we are one of the lucky families so far. No bereavements and financially we are secure compared to so many. I felt so guilty at not being able to ‘pull weight’ as I saw it. Being asthmatic I was nervous of volunteering to help, which is one of my drivers in life.
We both lost our three streams of income at once, with no guarantee that they were going to return. We went from a household of two to a household of six. Two adult children arrived home jobless, one bringing a jobless partner, and the third came back to sit online university exams with no guarantee of his third year going ahead. Uncertainly was rife. My husband then returned to hospital with an attack of Atrial fibrillation, a heart condition. Nothing to do with stress!? Things have since calmed down a bit, and we are one of the lucky families so far. No bereavements and financially we are secure compared to so many. I felt so guilty at not being able to ‘pull weight’ as I saw it. Being asthmatic I was nervous of volunteering to help, which is one of my drivers in life.


